There are advancements in the world of health care every minute it seems. With developments like backpack hearts and hybrid organ donations, it’s tough to know exactly what will emerge next. But, a wild new advancement is hitting the health care industry that could bring promising results to neonatal health care. Recently, fetal surgeon Dr. Alan Flake, director of the Center for Fetal Research in the Center for Fetal Diagnosis and Treatment at Children’s Hospital of Philadelphia, published research completed on artificial wombs for lambs born prematurely. With a successful run thus far, science may have an answer on how to give infants their much-need extra time in development.
How the Artificial Wombs Work
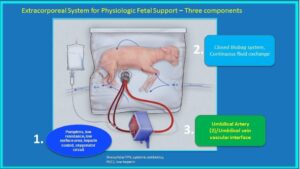
While the appearance of the artificial wombs may be strange and a bit jarring, they are closely replicating a natural placenta. Called the Biobag, the actual structure is similar to that of a giant Ziploc bag. The womb is a pumpless system made of polyethylene and uses tubes to circulate fluids containing electrolytes that would normally be found circulating through the mother’s veins into the placenta. The artificial wombs also reflect the functions of an actual placenta by filtering in oxygen.
(Courtesy of Children’s Hospital of Philadelphia)
During the research, the fetal lambs delivered around 100 to 115 days were placed in the Biobag. This amount of gestation time is similar to a baby being born around the 24-week point in human gestation. Once delivered, the lambs were immediately placed inside of the artificial wombs. During their time inside the Biobag, the lambs continued the process they normally would inside a natural womb. They continued breathing and swallowing amniotic fluid and moved around. The most important aspect researchers were looking for was growth among the 8 lambs placed in the bags.
Results
The lambs remained in the artificial wombs for 4 weeks after which they were “born.” Throughout their time in the bags, researchers noted the infants did not appear distressed, had room to move around, grew to the proper size and even grew wool. Their organ growth and maturation appeared stable and comparable to that of lambs born early and not placed in the Biobag.
Currently, the results from these artificial wombs cannot directly relate to usage for human infants. The average size of a newborn lamb is three times the size of a human infant. There is also no way of fully calculating the success and brain function in the lambs. The amniotic fluid would also need to be perfected for human use as well.
Why this is Important
The Biobag for human children would work under a routine C-section retrieving the premature baby from its mother and connecting the umbilical cords to the new system. When everything within the bag is flowing properly (fluids, oxygen, nutrients), the umbilical cord would then be detached from the artificial womb. Babies may not be carried to the typical full 40-weeks as in average human gestation, yet they would live in the Biobag until they can support themselves — still better than being born at 24-weeks or earlier.
The results from this research have shown great strides in determining the future of saving premature babies from death. Currently, 1 in 10 babies is born prematurely with this occurrence being the leading cause of death in infants. The minute a baby is born and take their first breath, their lungs inflate and their system stop relying on the mother for assistance. When a baby is born premature, their lungs, brain, physical structure and other essential systems can no longer develop. They are left to survive in the state at which they were born. The Biobag allows for an environment that more closely resembles a natural womb, especially compared to a ventilator and other machines in most neonatal intensive care units.
